Sleep Cycle: Quarterly Report #1
Raising sleep health awareness: How changes in behaviors and worries due to the pandemic are impacting sleep worldwide
Methodology:
The Sleep and Mental Health Amidst the 2020 Coronavirus Pandemic report is an analysis of global sleep patterns, behaviors and mental health issues related to the early months of the COVID-19 pandemic. The report draws on Sleep Cycle app data aggregated from over 33 million nights of users’ sleep between January and May 2020, tracking sleep quality. Additionally, 69,047 global Sleep Cycle users participated in an in-app survey designed to learn more about how changes in daily routine, mental health and worries related to the pandemic have affected sleep all around the world. The survey was deployed from June 17 to 22, 2020 in 22 countries, spanning North America, South America, Asia, Europe, Africa, Australia/New Zealand and the Middle East. Among the respondents, 95% reported being under stay-at-home orders at some point in the early stage of the pandemic.
Rebecca Robbins, PhD, Postdoctoral Fellow at Brigham and Women’s Hospital and Harvard Medical School collaborated with Sleep Cycle on this report.
Executive Summary:
The COVID-19 pandemic has fundamentally changed our lives in nearly every way, profoundly impacting the way we work, live, and our ability to sleep. For those fortunate to work from home, we now face less structure in our working lives and potentially more responsibilities, like caring for loved ones or children. Unfortunately, many have also lost their jobs or are working longer hours. In these uncertain times, sleep is likely to suffer. Sleep is a cornerstone of our health and well-being. Without healthy sleep, we are more prone toward negative mood, anxiety, and depression. In our analysis of Sleep Cycle data and user-reported health and well-being data, we identify the groups who are suffering from sleep issues and poor mental health. We demonstrate that our global population is experiencing adverse mental health consequences associated with COVID-19, such as more depressed mood and anxiety. Fortunately, we also identify easily modifiable behaviors that can pave the way toward better sleep during COVID-19, such as calming bedtime routines and cutting down on news exposure. Prioritizing sleep may be one of the most expedient pathways to mental and emotional health during troubling times. ~ Dr. Rebecca Robbins
What Was Keeping the World up at Night?

Key Takeaways From the onset of the pandemic:
- Teens and young adults got the worst sleep, had the highest rate of feeling depressed, experienced more loneliness and consumed too much technology as they transitioned to remote learning
- Across continents, age groups and genders, 37% of survey respondents reported taking longer to fall asleep, but women were twice as likely to take longer to fall asleep
- In our survey, almost half of respondents worldwide reported feeling more anxious, and almost a quarter felt more depressed
- People on every continent reported consuming too much news and too much technology, which contributed to sleep problems
No matter where you live in the world, people were worried about many of the same things when the outbreak began. We felt increased levels of anxiety and depression, and many of us had a harder time falling asleep than normal. Our survey paints a dire picture of how stress factors due to COVID-19 are impacting both our mental health and sleep habits.
It’s taking many of us longer to fall asleep during the pandemic
While many of us have been sleeping more during the pandemic — after all, we could sleep-in since we were no longer commuting to work or school — our global survey shows that 37% took longer to fall asleep.
Known as sleep onset latency, the period between being fully awake and asleep is critical to overall sleep health. A shorter sleep onset latency promotes a complete sleep cycle and is related to better sleep quality. The more stress we’re under, the longer our sleep latency can be. While there are many factors that may impact the amount of time it takes to fall asleep, such as bedtime and wake-up time, in this report, we focus on the psychological effects of the pandemic on sleep latency.
We asked survey participants whether they’ve noticed a change in how they fall asleep since the outbreak. See the graph below for the breakdown by region of those reporting longer sleep latency.
Sleep latency by region
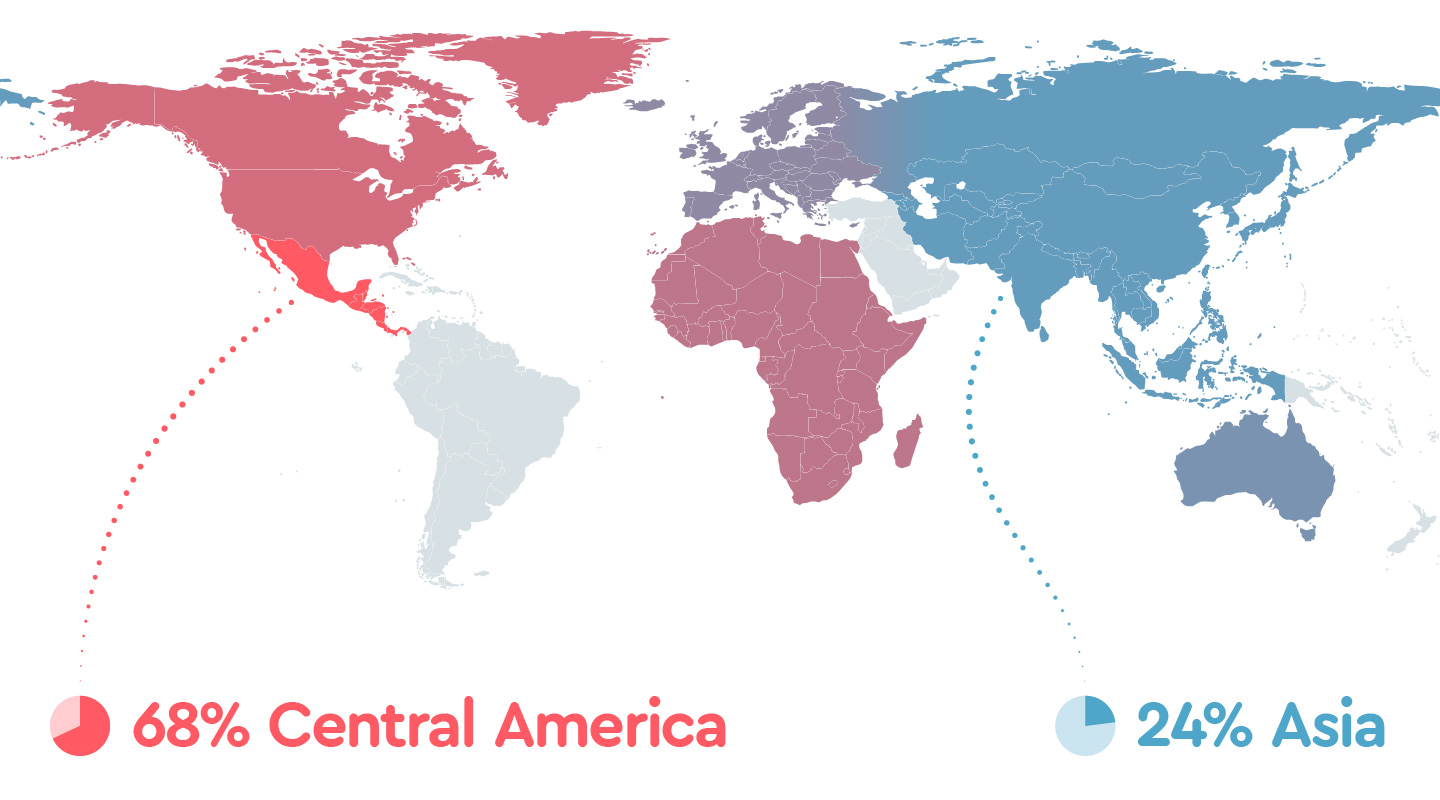
| 1.1 Longer sleep latency | |
|---|---|
| Central America | 68% |
| North America | 49% |
| Africa | 47% |
| Europe | 42% |
| Australia | 40% |
| Asia | 24% |
Women were twice as likely to have difficulty falling asleep than men.* In terms of their behaviors and primary concerns stemming from the pandemic, women and men around the world both reported consuming too much news and technology, but men were reportedly more worried about losing their job and/or personal finances while more women reported feeling anxious in general.

| 1.2 Longer sleep latency by sex | ||
|---|---|---|
| Women | 45% | |
| Men | 29% | |
* According to ordinal logistic regression analyses, using gender as a predictor, women were twice as likely to experience longer sleep latency
Teens and young adults felt the greatest impact on their sleep and happiness due to changes in daily routine, raising concerns about returning to remote learning this fall
Based on Sleep Cycle user data on sleep quality between January and May 2020 aggregated from over 33 million nights of sleep, we found that just as the virus was beginning to grip the world, the youngest age group in our database, people 18 to 24, had the lowest average sleep quality, globally. Not only did this population sleep the worst, but they also had the highest percentage of respondents who reported a longer sleep onset latency, more so than any other age group. Almost half of young adults in our survey experienced longer sleep latency.
Sleep latency by age group
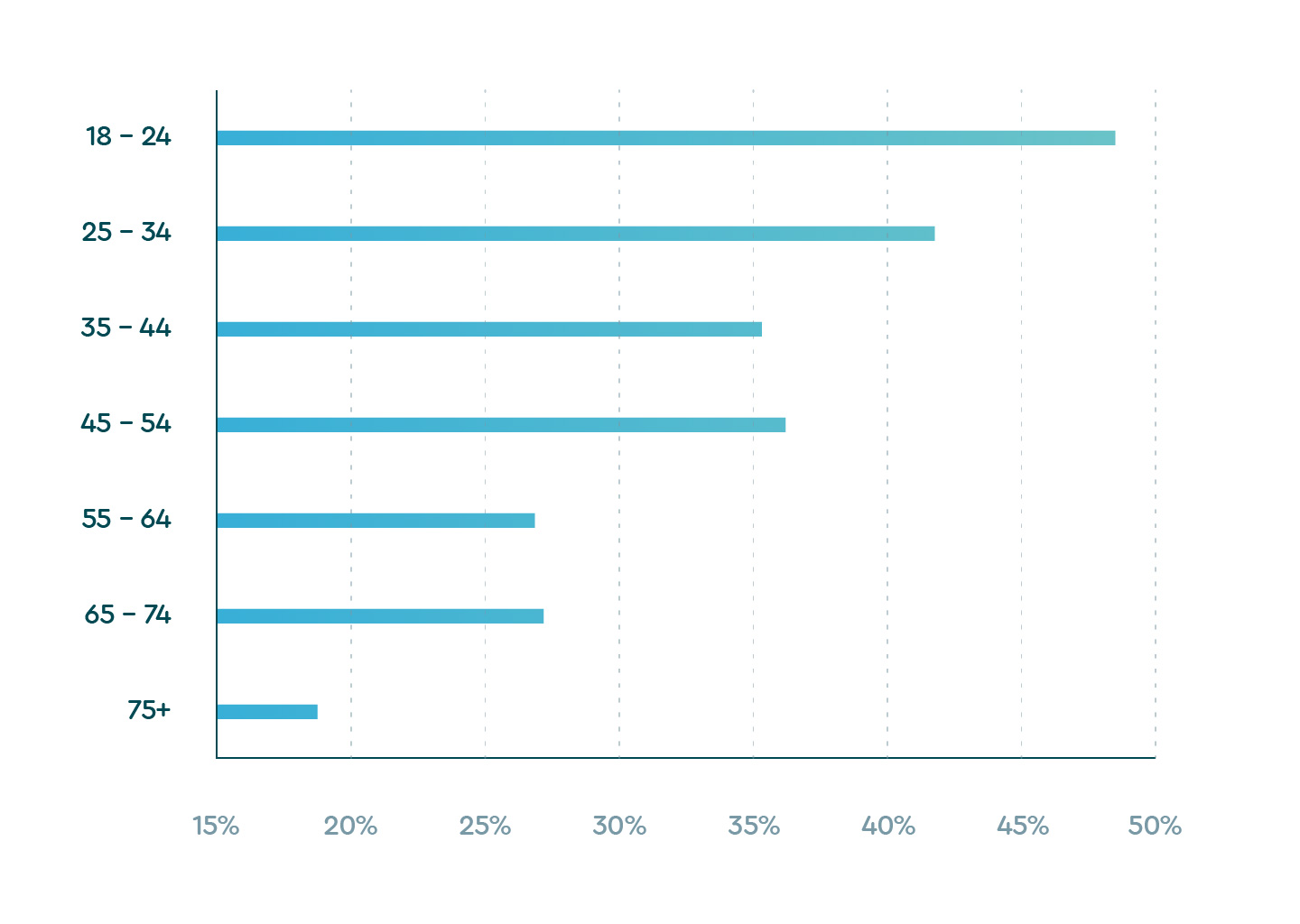
| 1.3 Reports of longer sleep latency by age | |
|---|---|
| 18 – 24 | 48.5% |
| 25 – 34 | 41.8% |
| 35 – 44 | 35.2% |
| 45 – 54 | 36.1% |
| 55 – 64 | 26.9% |
| 65 – 74 | 27.1% |
| 75+ | 18.8% |
Why did sleep health suffer so significantly for young people?

Much of it has to do with what they revealed about both their state of mind and the lifestyle changes thrust on them during the outbreak.
When we asked survey respondents how their daily routine has changed during COVID, the most prominent response for young people was “transitioned to remote learning” (15.02% or 7,801), followed by “commuting less” (14.67% or 7,617) and “spending less time in daylight” (13.76% or 7,145).
Over one-third (34.8%) of this age group reportedly felt “more depressed” since the pandemic, a larger percentage than any other age group. By comparison, only 18.5% of people in the groups most at-risk for illness, age 65 to 74, and 19.2% of people over 75, reported feeling more depressed.
Depression and anxiety
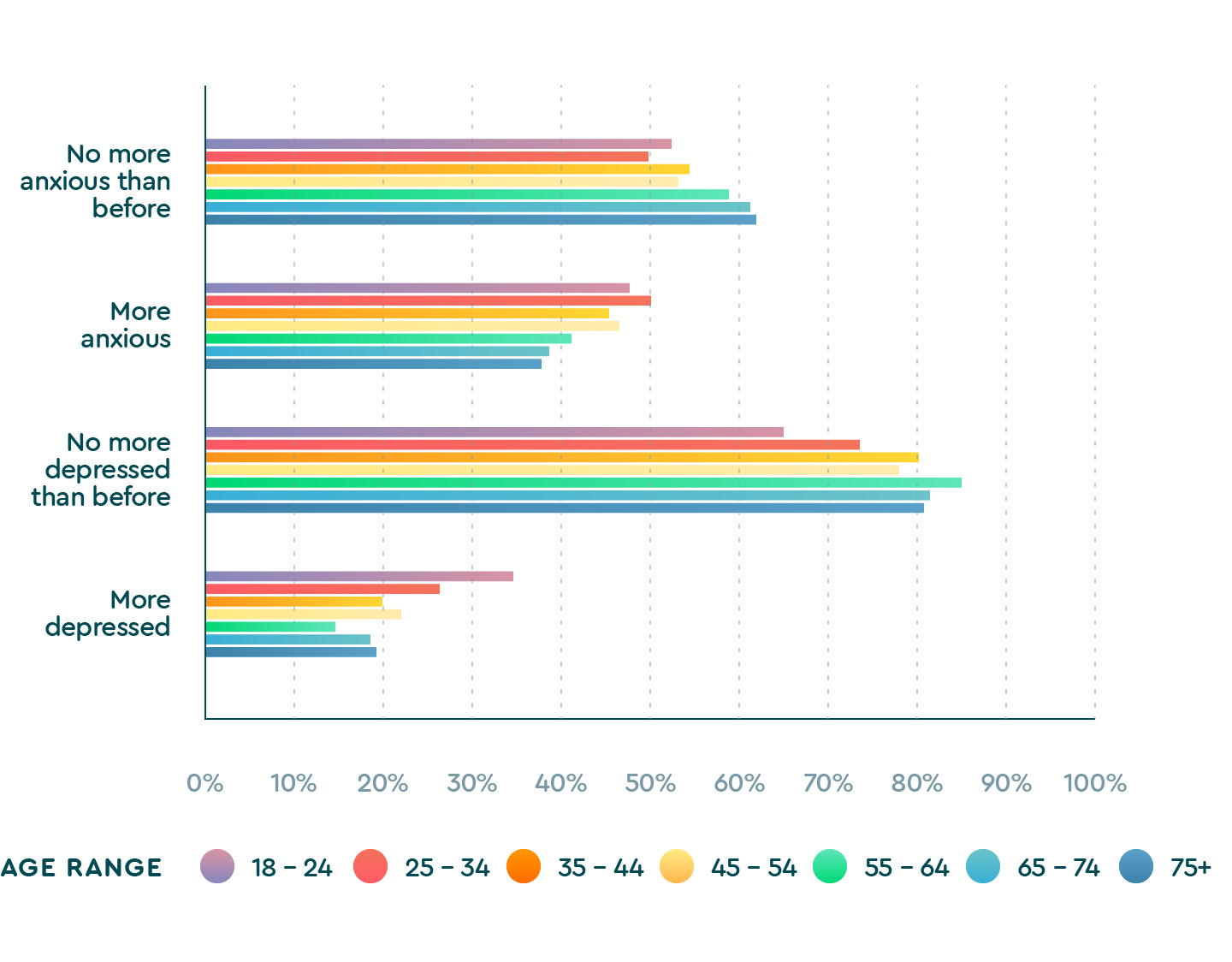
| 1.4.1 Age and depression and anxiety | ||
|---|---|---|
| Age groups | No more anxious than before | More anxious |
| 18 – 24 | 52.4% | 47.6% |
| 25 – 34 | 49.9% | 50.1% |
| 35 – 44 | 54.5% | 45.5% |
| 45 – 54 | 53.3% | 46.7% |
| 55 – 63 | 58.9% | 41.1% |
| 65 – 74 | 61.3% | 38.7% |
| 75+ | 62.0% | 38.0% |
| 1.4.2 Age and depression and anxiety | ||
|---|---|---|
| Age groups | No more depressed than before | More depressed |
| 18 – 24 | 65.2% | 34.8% |
| 25 – 34 | 73.5% | 26.5% |
| 35 – 44 | 80.1% | 19.9% |
| 45 – 54 | 77.9% | 22.1% |
| 55 – 64 | 85.2% | 14.8% |
| 65 – 74 | 81.5% | 18.5% |
| 75+ | 80.8% | 19.2% |
Younger people also felt the isolation and lack of socialization deeply. In our survey, it was the only age group that ranked “being lonely” as the primary worry on their minds. Loneliness in response to COVID-19 was the subject of a recent study by the American Psychological Association (APA) that surveyed 1,500 Americans age 18 to 98 and found, “Contrary to expectations, the social (physical) distancing recommendations and stay-at-home orders… did not lead to an uptick in loneliness among Americans.” APA researchers had predicted a rise in loneliness for at-risk groups such as elderly people living alone and those with chronic health conditions and were surprised to find the resiliency of those groups. Although we don’t have data on feelings of loneliness pre-pandemic, our survey of 69,047 global app users (16,982 of whom are 18 to 24 years old) indicates that younger people may be experiencing stay-at-home orders differently than the rest of the population. The long-term effects of social isolation on the mental health of teens and young adults is something to be watched as the pandemic rages on.

The second biggest thing troubling them was, “consuming too much technology.” Numerous studies show a correlation between excessive social media consumption (i.e. technology) and poor sleep habits in teens. Time spent on the phone or game console late at night competes for vital sleep hours, and blue light from screens is proven to block the release of melatonin, making sleep more difficult.
Transitioning to remote learning also impacted behavior in that this age group reported “spending less time in daylight.” Incidentally, they were the only age group to report time spent indoors as one of the top three changes in their daily routine. Exposure to the full spectrum of colors in natural light is important in controlling our sleep cycle, or circadian rhythm, and the lack of time spent outdoors impedes sleep.
Top worries by age
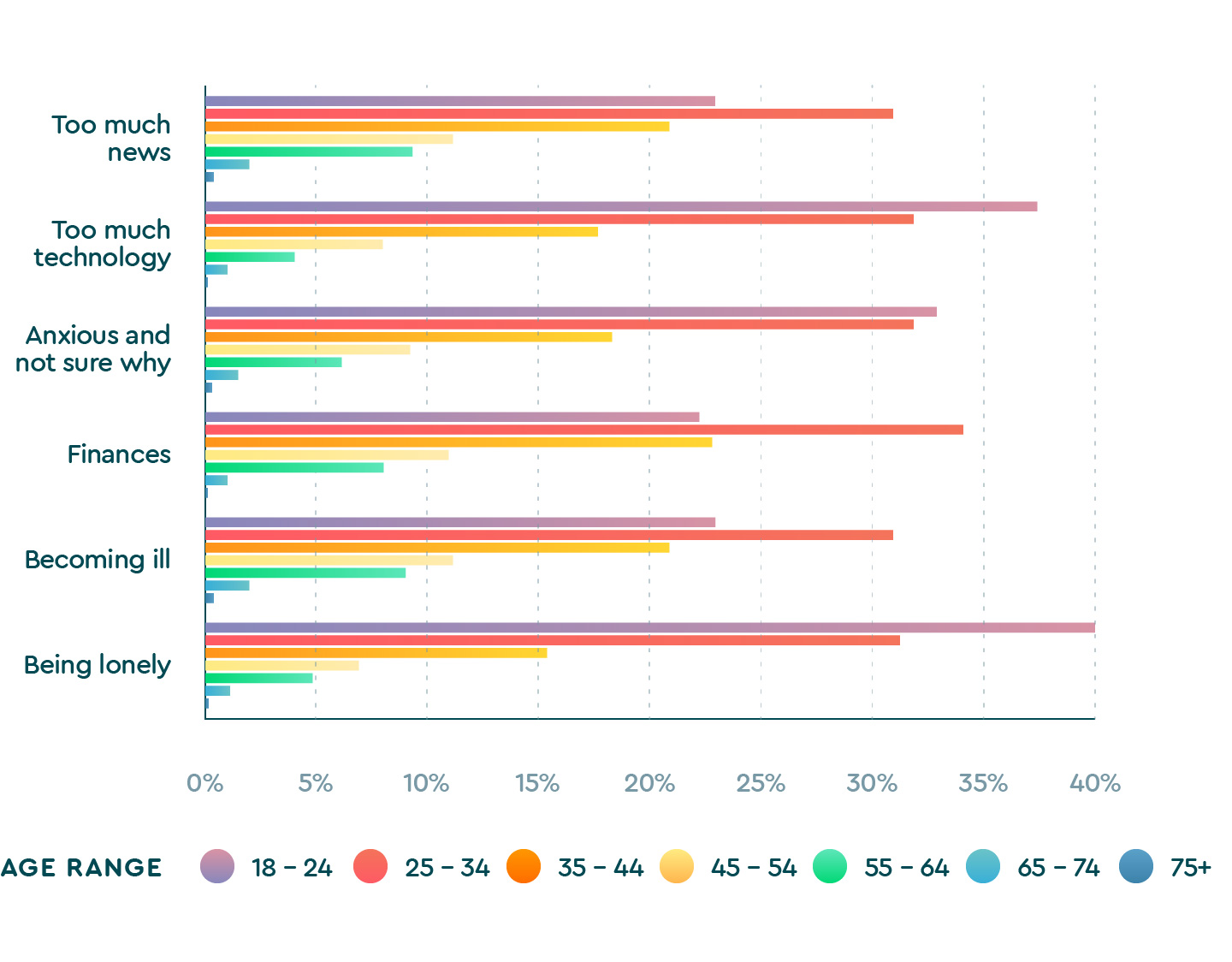
| 1.5.1 Top worries by age | |||
|---|---|---|---|
| Age groups | Too much news | Too much technology | Anxious and not sure why |
| 18 – 24 | 23.5% | 38.1% | 33.0% |
| 25 – 34 | 31.0% | 31.9% | 32.0% |
| 35 – 44 | 21.4% | 16.9% | 17.5% |
| 45 – 54 | 11.6% | 7.9% | 9.3% |
| 55 – 64 | 9.6% | 4.2% | 6.3% |
| 65 – 74 | 2.6% | 1.0% | 1.6% |
| 75+ | 0.4% | 0.2% | 0.3% |
| 1.5.2 Top worries by age | |||
|---|---|---|---|
| Age groups | Finances | Becoming ill | Being lonely |
| 18 – 24 | 22.7% | 23.5% | 40.1% |
| 25 – 34 | 34.2% | 31.0% | 31.4% |
| 35 – 44 | 22.9% | 21.4% | 15.3% |
| 45 – 54 | 11.2% | 11.6% | 6.9% |
| 55 – 64 | 7.9% | 9.6% | 4.8% |
| 65 – 74 | 1.0% | 2.6% | 1.3% |
| 75+ | 0.1% | 0.4% | 0.2% |
Our survey paints a troubling picture for young people. Staying home instead of being in school, young adults around the world were isolated from social activity. They stayed inside, got less sunlight and turned to technology. They experienced heightened feelings of depression, anxiety and loneliness, more so than any other age group. And, across the board, young adults slept the worst.
For parents, educators and younger populations, this is a critical moment for sleep health awareness. Sleep is a function of what we do during the day, not just our bedtime routines. Whether students return to school or continue to learn from home, there are many small behavioral changes they should incorporate into their daily lives to get a restful sleep, starting from the moment they wake up. Here are some fundamental ways to promote healthy sleep and add structure to the day:
- Break a sweat
- Get fresh air
- Manage stress
- Put the phone away an hour before bedtime
Spike in feelings of anxiety and depression
With the heightened fear, stress and uncertainty around COVID, we wanted to find out what impact the pandemic has had on our mental health in general. It’s been reported, most notably by the National Center for Health Statistics in conjunction with the U.S. Census Bureau, that one-third of Americans are showing signs of clinical anxiety and depression because of COVID-19. Our survey asked participants if they were experiencing an increase, decrease, unknown or no change in feelings of anxiety and depression since the pandemic, and the responses indicate that number could be higher on a global scale. Among the overall survey sample, nearly half of respondents (44.5%) reported feelings of more anxiety during COVID-19 and about a quarter (23.5%) reported feelings of more depression.
Additionally, people who reported feeling more anxious and/or depressed, also experienced a longer sleep latency. In fact, people who reported difficulty falling asleep during the pandemic were almost three times more likely to report greater feelings of anxiety and approximately two times more likely to report greater feelings of depression.
The duration of the sleep latency is also telling. Among those who reported preexisting mental health concerns and taking longer to fall asleep, the vast majority (85.5% with anxiety; 83% with depression) took 30 minutes or more than usual to fall asleep.
Our sleep is directly related to our mental health. After a night of insufficient or poor-quality sleep, we wake up and are more prone to negative mood states, including irritability, anxiety and depression. We are also less able to engage in ‘perspective taking,’ or, in other words, put negative experiences, conversations, or events in context. Thus, poor sleep can trigger a negative spiral. Conversely, keeping a healthy sleep schedule can contribute to a positive spiral, whereby healthier sleep contributes to a more positive outlook and creates a buffer against negative mood, anxiety and depression. Our survey found that people experiencing longer sleep latency were at greater risk for mental health concerns.
Mental health and sleep latency
| 1.6 Sleep latency and mental health | ||||
|---|---|---|---|---|
| How much longer does it take you to fall asleep? | ||||
| A few minutes | 30 minutes or more | |||
| More anxious | 17.0% | 85.5% | ||
| More depressed | 14.5% | 83.0% | ||
Certain stress factors and daily habits are causing sleep difficulty
The stress the world feels from the pandemic is weighing on all of us and carrying over into our sleep. We asked survey participants to identify all the factors that have impacted their ability to fall or stay asleep since the outbreak. Three trends emerged: people are consuming too much technology, too much news and generally feel more anxious without being able to pinpoint a specific reason.
Top worries around the world
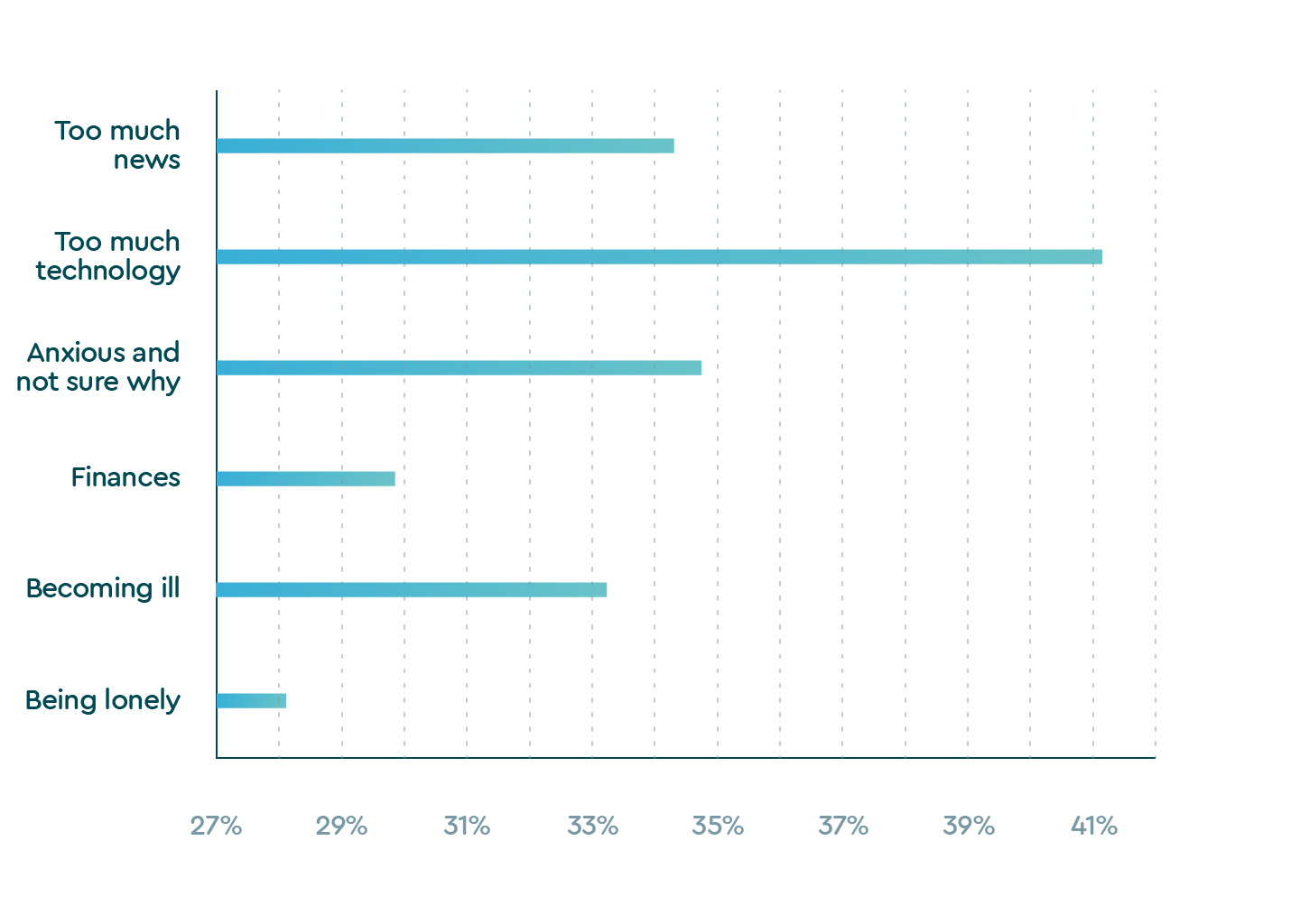
| 1.7 Top worries around the world | |
|---|---|
| Too much technology | 41.2% |
| Anxious and not sure why | 34.8% |
| Finances | 29.8% |
| Becoming ill | 33.2% |
| Being lonely | 28.1% |
Concerns over finances was the thing keeping most working-age people up at night, and it’s no surprise. With global economies halted and unemployment rates hitting record highs, respondents aged 25-44 ranked “I’m worried about my job and/or personal finances” as their primary stress factor. People aged 45-64 ranked it in their top three worries. Overall, about one-third of respondents reported finances as one of their top worries and were 1.8 times more likely to report difficulty falling asleep. Those who lost their job were at a much greater risk for sleep difficulty.
Fear of becoming ill or having a loved one fall ill was on the minds of people age 35 and older, who marked it in their top three worries. (See Health Care section below for more on this.) This stress factor correlates to being 1.4 times more likely to report difficulty falling asleep.
Many facets of our everyday life and daily behaviors also changed and coincided with what we perceive as our ability to fall asleep. Our results show that drinking more alcohol and caffeine, consuming more technology and getting less exercise all put us at great risk for taking longer to fall asleep.
Top worries among those taking longer to fall asleep
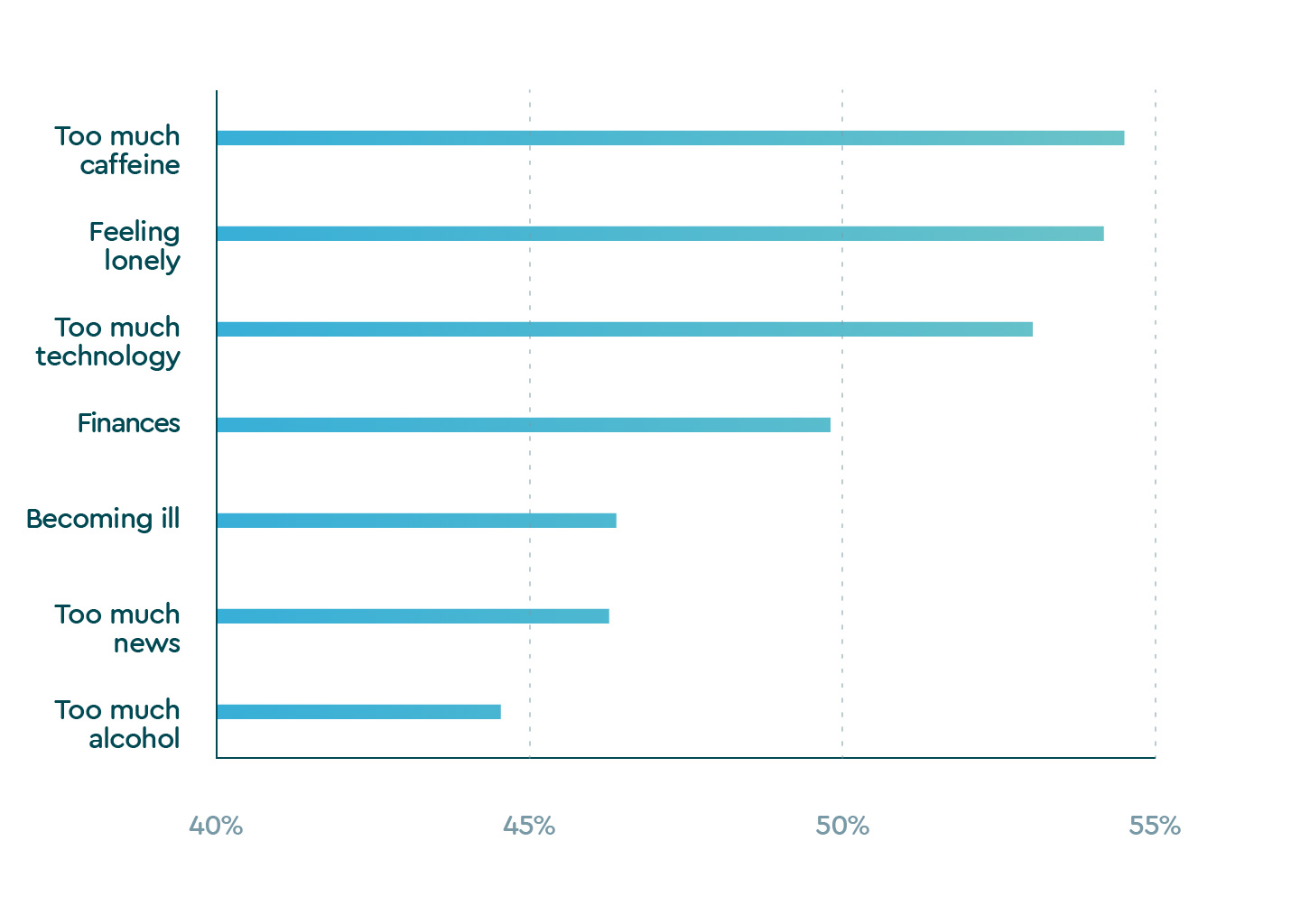
| 1.8 Top worries among those taking longer to fall asleep | |
|---|---|
| Too much caffeine | 54.5% |
| Feeling lonely | 54.1% |
| Too much technology | 53.4% |
| Finances | 49.8% |
| Becoming ill | 46.4% |
| Too much news | 46.4% |
| Too much alcohol | 44.6% |
Who Slept Best (and Worst) During the Pandemic?
Key Takeaways
- Older people (ages 65 to 74) had the highest sleep quality from January to May
- Around the world, people exercised less in the early months of the pandemic
- Respondents in North America, Europe and Australia reported consuming more alcohol
While every person faces their own unique challenges because of coronavirus, the pandemic has forced most of us to restructure our daily routines on a global scale we’ve never experienced. At Sleep Cycle, we wanted to find out how sleep quality was affected during the early months of the pandemic and if there were any common threads around the world in how daily life and behaviors changed.
Being well physically, mentally and emotionally requires sleep. And, it’s not just about duration. Seven to eight hours of fitful sleep per night filled with bouts of wakefulness doesn’t give our bodies and brains the recovery time needed for good health. We need the deeper, restorative phases of sleep in order to wake up feeling refreshed. Sleep quality matters.
The Sleep Cycle app quantifies sleep quality based on factors including sleep duration, restfulness and movements during sleep. We looked at the data to see who got the best and worst sleep quality around the world during the beginning of the pandemic, but we also wanted to understand why, so in our survey we asked how life changed.
The most vulnerable age group (65 to 74) slept the best
As we pointed out, the youngest age group had the poorest sleep quality between January and May 2020. Surprisingly, the oldest age group in our database (65 to 74) had the highest sleep quality. Why would the group who’s at greatest risk of complications and mortality from the virus sleep best? One explanation is that they simply weren’t plugged in to technology the way younger generations said they were. Perhaps with more life experience comes more perspective.
Sleep quality globally by age group between January and May 2020
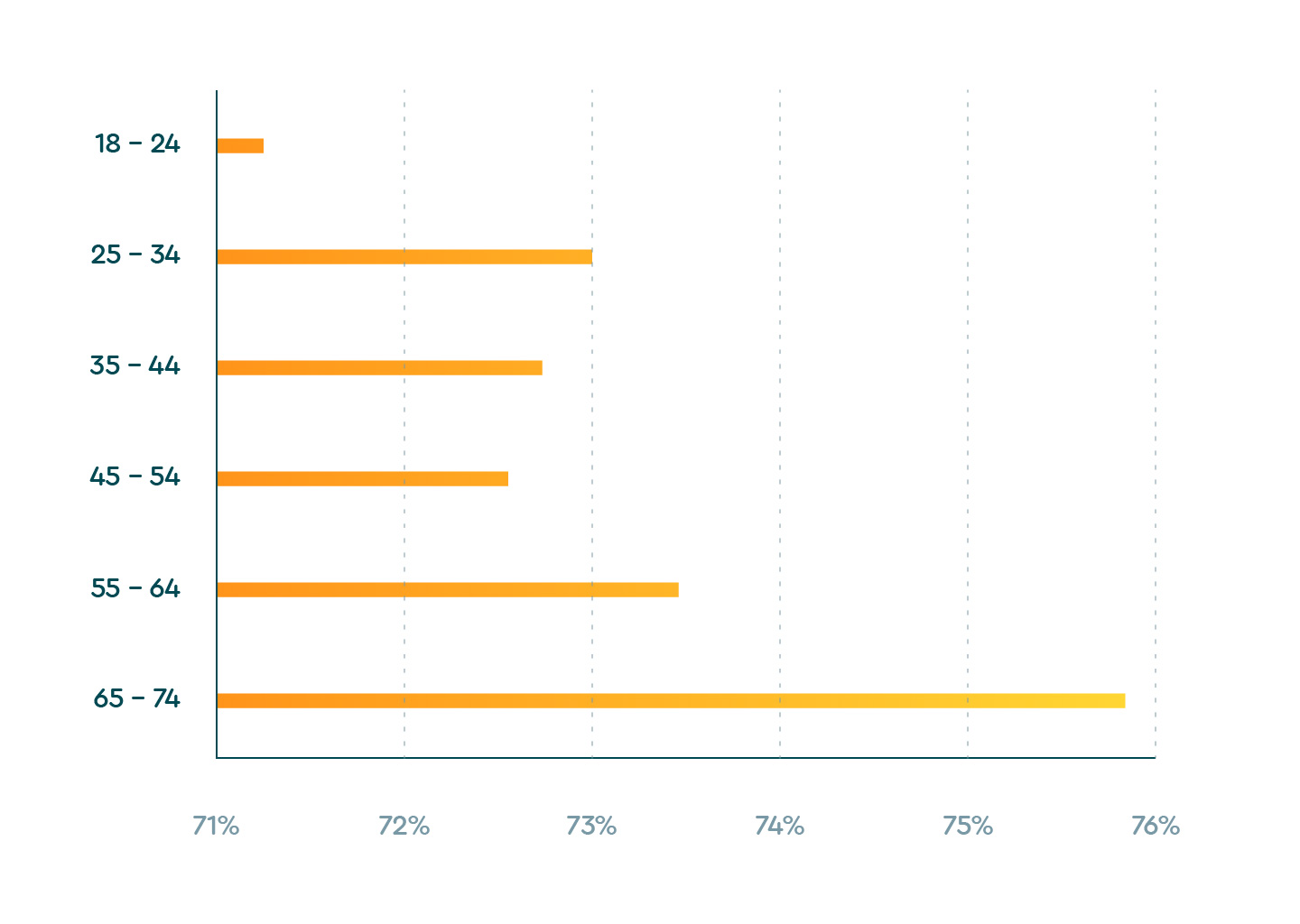
| 2.1 Age Range and Average Sleep Quality | |
|---|---|
| 18 – 24 | 71.3% |
| 25 – 34 | 73.0% |
| 35 – 44 | 72.8% |
| 45 – 54 | 72.5% |
| 55 – 64 | 73.4% |
| 65 – 74 | 75.7% |
Based on Sleep Cycle app data aggregated over 33,619,126 nights
We also pulled data from around the world to find out which countries had the highest and lowest sleep quality. Brazil, Japan and South Korea scored the worst, while Belgium, the United Kingdom and Sweden sleep best.
Which countries slept best (and worst) between January and May 2020?
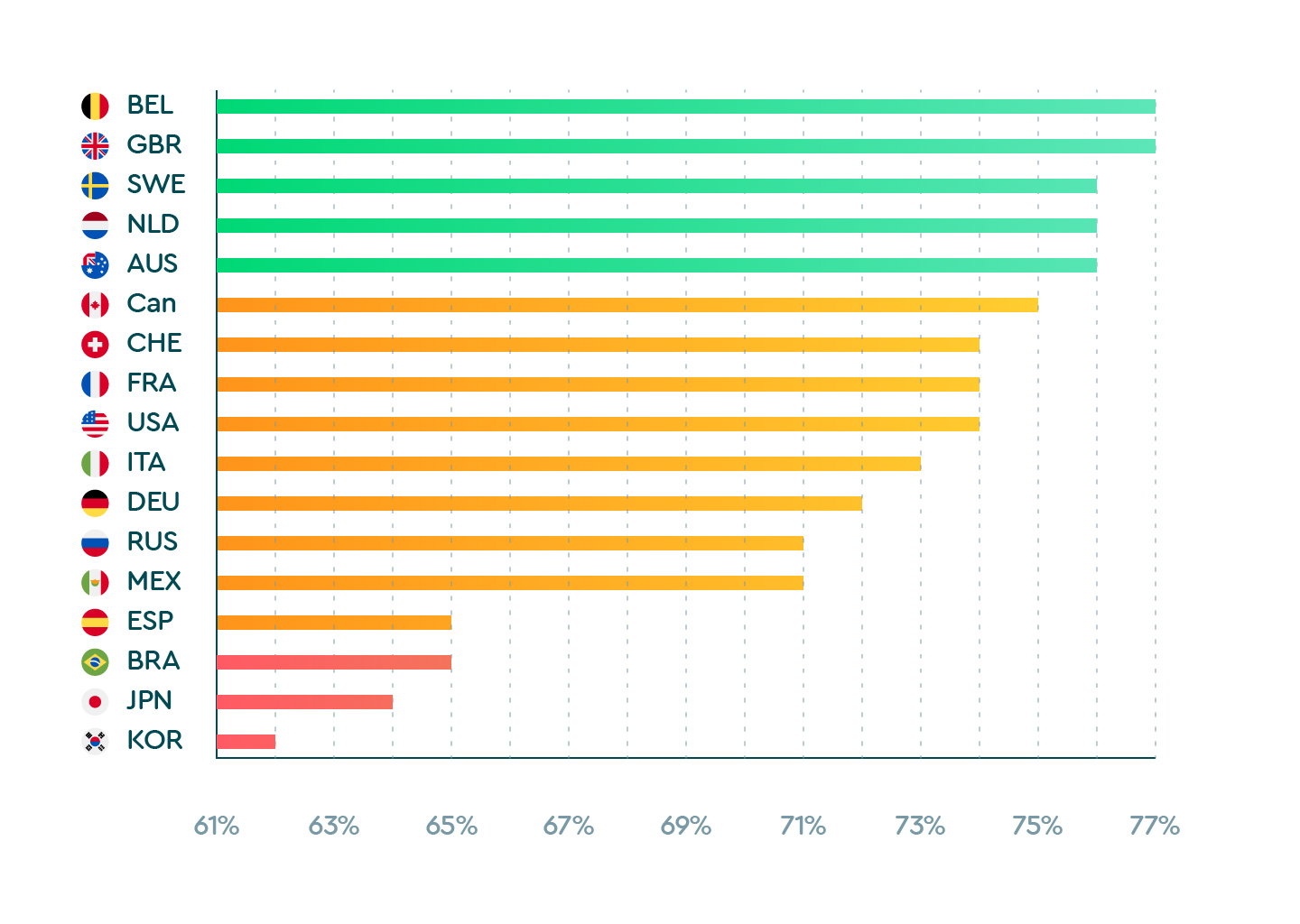
| 2.2 Which countries slept best (and worse) between January and May 2020? | |
|---|---|
| Belgium | 77% |
| United Kingdom | 77% |
| Sweden | 76% |
| Netherlands | 76% |
| Australia | 76% |
| Canada | 75% |
| Switzerland | 74% |
| France | 74% |
| United States | 74% |
| Italy | 73% |
| Germany | 72% |
| Russia | 70% |
| Mexico | 70% |
| Spain | 65% |
| Brazil | 65% |
| Japan | 64% |
| South Korea | 62% |
Based on Sleep Cycle app data aggregated over 33,400,875 nights
How life changed around the world

Getting a good night’s rest starts the moment we wake up. As we approach bedtime, nighttime routines can help set the groundwork for good sleep, but sleep quality is also a function of what we do over the course of the day. Managing stress and having structure in our lives is critical for sleep.
The rampant spread of the virus forced us to make drastic changes to work environments, social interactions, business operations, and school activity. Most of us were put under some form of stay-at-home order for the first time in our lives. What effects did that have on our sleep?
We asked app users to tell us the ways in which their lives have changed since the outbreak. Working from home, transitioning to remote learning, commuting less, and exercising less emerged as universal changes to daily routines worldwide.
| Africa’s top 3 routine changes | |
|---|---|
| Working from home | 60.14% |
| Working fewer hours | 23.67% |
| Working more hours | 30.58% |
| Lost my job, now unemployed | 5.32% |
| Transitioned to remote learning | 22.31% |
| Spending more time helping my children with schoolwork | 10.31% |
| Spending more time taking care of children | 12.80% |
| Commuting less | 57.08% |
| Commuting more | 1.93% |
| Exercising more | 19.82% |
| Exercising less | 45.07% |
| Spending more time in daylight | 11.89% |
| Spending less time in daylight | 36.58% |
| No changes | 4.64% |
| Africa’s alcohol consumption | |
|---|---|
| No change | 29.25% |
| I’m drinking less | 26.60% |
| I’m drinking more | 17.46% |
| I don’t drink alcohol | 26.01% |
| I haven’t noticed a change | 0.69% |
| Asia’s top 3 routine changes | |
|---|---|
| Working from home | 34.78% |
| Working fewer hours | 24.525% |
| Working more hours | 9.65% |
| Lost my job, now unemployed | 1.59% |
| Transitioned to remote learning | 8.99% |
| Spending more time helping my children with schoolwork | 3.58% |
| Spending more time taking care of children | 7.90% |
| Commuting less | 30.38% |
| Commuting more | 1.09% |
| Exercising more | 9.03% |
| Exercising less | 44.13% |
| Spending more time in daylight | 5.16% |
| Spending less time in daylight | 34.17% |
| No changes | 16.82% |
| Asia’s alcohol consumption | |
|---|---|
| No change | 35.35% |
| I’m drinking less | 12.28% |
| I’m drinking more | 19.66% |
| I don’t drink alcohol | 29.74% |
| I haven’t noticed a change | 2.97% |
| Australia’s top 3 routine changes | |
|---|---|
| Working from home | 44.67% |
| Working fewer hours | 20.81% |
| Working more hours | 24.06% |
| Lost my job, now unemployed | 9.64% |
| Transitioned to remote learning | 21.93% |
| Spending more time helping my children with schoolwork | 6.90% |
| Spending more time taking care of children | 8.32% |
| Commuting less | 51.78% |
| Commuting more | 3.15% |
| Exercising more | 22.23% |
| Exercising less | 42.94% |
| Spending more time in daylight | 10.56% |
| Spending less time in daylight | 34.01% |
| No changes | 8.73% |
| Australia’s alcohol consumption | |
|---|---|
| No change | 32.47% |
| I’m drinking less | 14.89% |
| I’m drinking more | 31.95% |
| I don’t drink alcohol | 20.37% |
| I haven’t noticed a change | 0.31% |
| Caribbean’s top 3 routine changes | |
|---|---|
| Working from home | 25.00% |
| Working fewer hours | 25.00% |
| Working more hours | 8.33% |
| Lost my job, now unemployed | 0.00% |
| Transitioned to remote learning | 4.17% |
| Spending more time helping my children with schoolwork | 16.67% |
| Spending more time taking care of children | 8.33% |
| Commuting less | 25.00% |
| Commuting more | 0.00% |
| Exercising more | 20.83% |
| Exercising less | 37.50% |
| Spending more time in daylight | 16.67% |
| Spending less time in daylight | 37.50% |
| No changes | 8.33% |
| Caribbean’s alcohol consumption | |
|---|---|
| No change | 38.10% |
| I’m drinking less | 4.76% |
| I’m drinking more | 28.57% |
| I don’t drink alcohol | 23.81% |
| I haven’t noticed a change | 4.76% |
| Central America’s top 3 routine changes | |
|---|---|
| Working from home | 47.37% |
| Working fewer hours | 23.55% |
| Working more hours | 21.88% |
| Lost my job, now unemployed | 7.20% |
| Transitioned to remote learning | 26.04% |
| Spending more time helping my children with schoolwork | 5.54% |
| Spending more time taking care of children | 7.48% |
| Commuting less | 21.05% |
| Commuting more | 2.22% |
| Exercising more | 32.13% |
| Exercising less | 31.86% |
| Spending more time in daylight | 13.02% |
| Spending less time in daylight | 31.30 % |
| No changes | 5.26% |
| Central America’s alcohol consumption | |
|---|---|
| No change | 29.26% |
| I’m drinking less | 13.35% |
| I’m drinking more | 21.59% |
| I don’t drink alcohol | 35.80% |
| I haven’t noticed a change | 0% |
| Europe’s top 3 routine changes | |
|---|---|
| Working from home | 47.46 |
| Working fewer hours | 21.87% |
| Working more hours | 21.18% |
| Lost my job, now unemployed | 5.05% |
| Transitioned to remote learning | 17.66% |
| Spending more time helping my children with schoolwork | 6.64% |
| Spending more time taking care of children | 9.39% |
| Commuting less | 45.42% |
| Commuting more | 1.62% |
| Exercising more | 29.77% |
| Exercising less | 32.59% |
| Spending more time in daylight | 23.02% |
| Spending less time in daylight | 22.00% |
| No changes | 7.77% |
| Europe’s alcohol consumption | |
|---|---|
| No change | 30.49% |
| I’m drinking less | 17.50% |
| I’m drinking more | 25.68% |
| I don’t drink alcohol | 19.72% |
| I haven’t noticed a change | 6.60% |
| North America’s top 3 routine changes | |
|---|---|
| Working from home | 51.87% |
| Working fewer hours | 22.92% |
| Working more hours | 23.38% |
| Lost my job, now unemployed | 9.52% |
| Transitioned to remote learning | 24.82% |
| Spending more time helping my children with schoolwork | 8.61% |
| Spending more time taking care of children | 12.13% |
| Commuting less | 55.32% |
| Commuting more | 2.52% |
| Exercising more | 28.24% |
| Exercising less | 39.80% |
| Spending more time in daylight | 23.46% |
| Spending less time in daylight | 29.26% |
| No changes | 5.19% |
| North America’s alcohol consumption | |
|---|---|
| No change | 32.06% |
| I’m drinking less | 10.95% |
| I’m drinking more | 32.33% |
| I don’t drink alcohol | 24.65% |
| I haven’t noticed a change | 0.01% |
| Pacific Island’s top 3 routine changes | |
|---|---|
| Working from home | 21.19% |
| Working fewer hours | 25.17% |
| Working more hours | 13.25% |
| Lost my job, now unemployed | 2.65% |
| Transitioned to remote learning | 11.26% |
| Spending more time helping my children with schoolwork | 4.64% |
| Spending more time taking care of children | 6.62% |
| Commuting less | 19.21% |
| Commuting more | 1.32% |
| Exercising more | 5.96% |
| Exercising less | 43.05% |
| Spending more time in daylight | 4.64% |
| Spending less time in daylight | 27.15% |
| No changes | 21.85% |
| Pacific Island’s alcohol consumption | |
|---|---|
| No change | 36.67% |
| I’m drinking less | 9.33% |
| I’m drinking more | 20% |
| I don’t drink alcohol | 32.67% |
| I haven’t noticed a change | 1.33% |
| South America’s top 3 routine changes | |
|---|---|
| Working from home | 32.79% |
| Working fewer hours | 18.03% |
| Working more hours | 21.31% |
| Lost my job, now unemployed | 6.56% |
| Transitioned to remote learning | 21.21% |
| Spending more time helping my children with schoolwork | 6.56% |
| Spending more time taking care of children | 11.48% |
| Commuting less | 32.79% |
| Commuting more | 3.28% |
| Exercising more | 27.87% |
| Exercising less | 27.87% |
| Spending more time in daylight | 9.84% |
| Spending less time in daylight | 22.95% |
| No changes | 9.84% |
| South America’s alcohol consumption | |
|---|---|
| No change | 34.48% |
| I’m drinking less | 10.34% |
| I’m drinking more | 17.24% |
| I don’t drink alcohol | 37.93% |
| I haven’t noticed a change | 0% |
| Other’s top 3 routine change | |
|---|---|
| Working from home | 23.74% |
| Working fewer hours | 23.64% |
| Working more hours | 10.61% |
| Lost my job, now unemployed | 2.03% |
| Transitioned to remote learning | 10.61% |
| Spending more time helping my children with schoolwork | 4.46% |
| Spending more time taking care of children | 8.53% |
| Commuting less | 18.22% |
| Commuting more | 1.41% |
| Exercising more | 10.17% |
| Exercising less | 32.7% |
| Spending more time in daylight | 6.59% |
| Spending less time in daylight | 27.08% |
| No changes | 22.04% |
| Other’s alcohol consumption | |
|---|---|
| No change | 41.75% |
| I’m drinking less | 8.28% |
| I’m drinking more | 19.53% |
| I don’t drink alcohol | 29.25% |
| I haven’t noticed a change | 1.19% |
Globally, respondents mostly reported no change in their alcohol consumption, with a few exceptions. North America, Europe and Australia all had significant groups of respondents who reported consuming more alcohol since the pandemic, as well as significant populations with no change in drinking behavior. Africa was the only region where alcohol consumption was down.
While the myth that a nightcap before bed can help you fall asleep still abounds, the scientific literature tells a different story. Alcohol pulls us out of deeper states of sleep and results in awakenings throughout the night, which leads to sleep that’s not restorative.
One of the more surprising findings in our survey was that, across the board, people exercised less. This is likely due to lockdowns leading to the closure of gyms, parks and outdoor recreational spaces. South America was the only region of the world in which respondents reported exercising more.
How does this impact sleep? Simply put, people who exercise get more, better quality sleep. In this time of social distancing and working-from-home, exercising in the living room or kitchen instead of going to the gym can be particularly difficult, and will require creativity. Finding small ways to break a sweat — whether it’s a set of push-ups or jumping jacks — is one of the fastest ways to a better sleep.
Healthcare Workers Had a Hard Time Falling Asleep

Key Takeaways
- Health care workers reported having more difficulty falling asleep since the pandemic than their peers
- The top worry on the minds of health care workers was becoming ill, or having a loved one fall ill
Health care workers have emerged as the heroes of this crisis. As the world was stretched thin on resources, we called on our nurses, doctors and long-term care providers to work grueling hours under difficult circumstances, often putting their own health at risk to care for COVID-19 patients. Particularly in the early months of the virus when governments and the private sector were struggling with supply chain disruption and shortages of critical personal protective equipment (PPE), health care workers didn’t have the luxury of staying home. They showed up for work.
And it took a toll on their sleep health
Overall, 39.1% of health care workers surveyed reported that it took them longer to fall asleep than before the pandemic. By comparison, 35.30% of their peers in the general population aged 35 to 44, reported difficulty falling asleep. (The median age of health care workers in the U.S. is 42.7 according to the Bureau of Labor Statistics.) Of those health care workers, most reported a sleep latency of 30 minutes longer. An even more concerning trend is the number of health care workers who, on average, took more than an hour to fall asleep.
Among health care workers reporting longer sleep latency, 81.7% reported taking 30 minutes or longer than usual to fall asleep
Why is this so concerning? On average, it takes about 15 to 20 minutes to fall asleep. Taking an additional hour or more beyond the average latency cuts short the total sleep duration for the night. The extraordinary stress health care workers experience on the job is, in many cases, causing them to lie in bed awake at night.
And they were more worried about becoming ill than the rest of us
Overall, 41.2% said their top worry was becoming ill or having a loved one become ill, which was tied for top place with “consuming too much news.” It shouldn’t come as a surprise that the stress of being on the front lines, caring for sick patients and seeing the seriousness of the illness day in and day out, caused health care workers to worry about their own health.
Conclusion
We looked at sleep from over 33 million nights of data and heard from over 69,000 global app users on how their daily routines, mental health and sleep have changed during the pandemic. Our research shows that teens and young adults are experiencing serious consequences to their sleep health. Transitioning to remote learning and social isolation has coincided with less time spent outside, less exercise, increased technology consumption, feelings of loneliness, depression and anxiety, as well as difficulty falling asleep. We showed that people around the world are experiencing longer sleep onset latency. In looking at mental health, we demonstrated that nearly half of our respondents are presenting increased feelings of depression and are overwhelmingly consuming too much technology. We identified lack of exercise and increased alcohol consumption as behaviors that are contributing to sleep problems in the COVID era. We explored the unique situation of health care workers, finding that they are at risk for sleep difficulty.
Given the cumulative negative effects on sleep worldwide that we’ve seen in the early stage of the pandemic, particularly among teens, young adults and health care workers, more focus needs to be given to understanding who is at risk and why. With the long tail of coronavirus still unknown, now is a critical time to raise awareness around sleep health and to promote healthy routines.
About Sleep Cycle
Sleep Cycle is the world’s most popular intelligent alarm clock app that analyzes users’ sleep, records findings and wakes them during their lightest sleep phase so they feel rested and refreshed. The app generates nightly sleep reports, tracks long-term sleep trends, and logs how daily activities impact sleep quality. With millions of users worldwide, Sleep Cycle has become the world’s richest repository of data on global sleep habits.
All Sleep Cycle sleep data used in this report is voluntarily shared anonymously by Sleep Cycle users. Sleep Cycle users can choose to decline or participate at any time. The data of users who decline participation is never shared or used for Sleep Cycle sleep research reports. User data remains safe and private, locally stored on the device, and in their online backup.

 What Was Keeping the World up at Night?
What Was Keeping the World up at Night?  Who Slept Best (and Worst) During the Pandemic
Who Slept Best (and Worst) During the Pandemic  Healthcare Workers Had a Hard Time Falling Asleep
Healthcare Workers Had a Hard Time Falling Asleep