Restless legs syndrome (RLS), also known as Willis–Ekbom disease, is a common sleep disorder that affects around 5% of the general population and as many as 10% of people over 65 years old. Here are 8 key things you should know if you suspect that you or someone you know may have RLS.
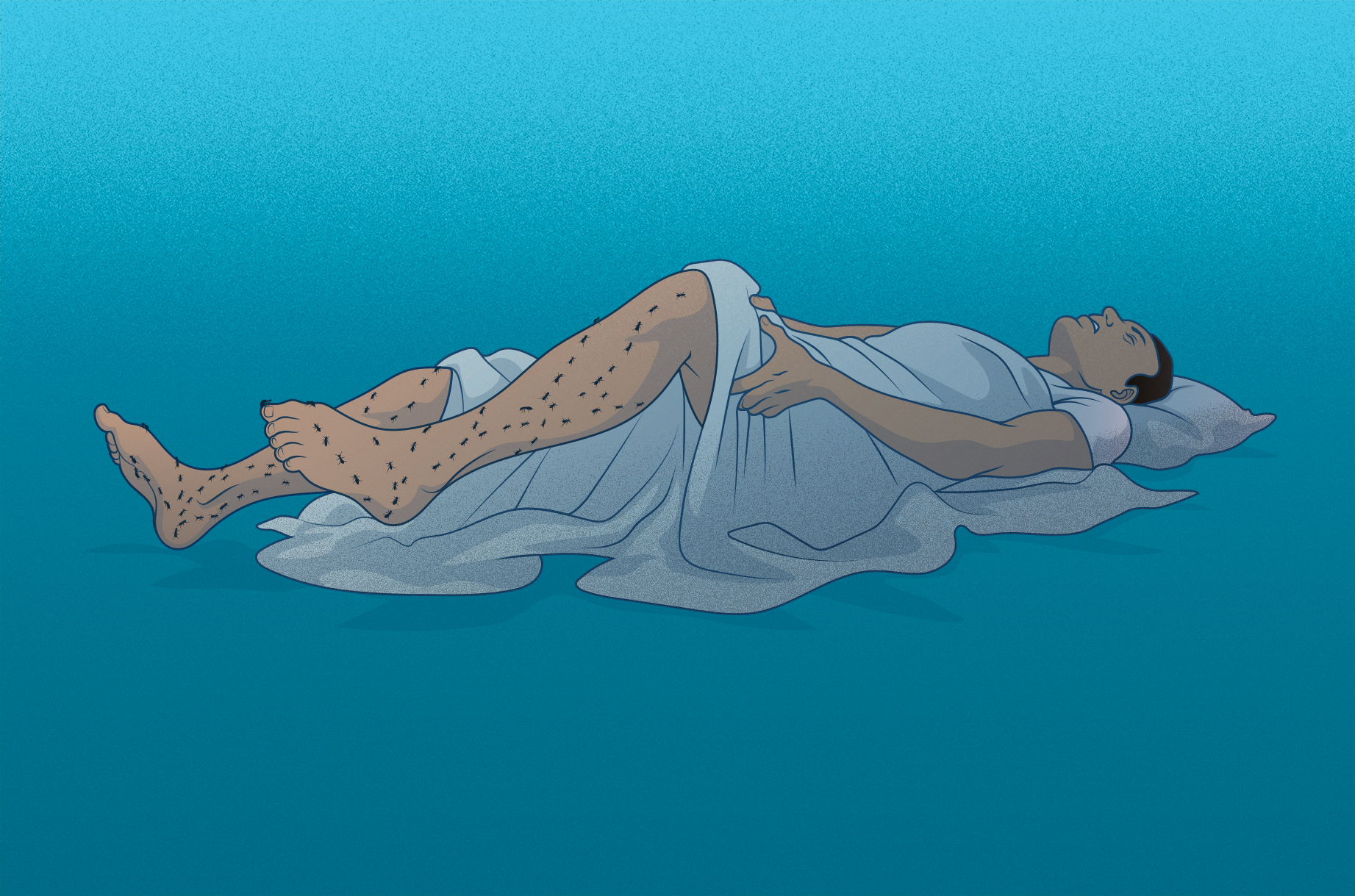
1. The exact symptoms vary widely
What it feels like to have RLS varies greatly – from a slight sense of discomfort to feelings of pain that give you an urge or a need to move your body, most often your legs. Episodes also vary in frequency. In severe cases of RLS, symptoms occur more than twice a week and seriously disrupt both your sleep and daily life, causing restless days and often sleepless nights.
2. Restless Legs Syndrome can also affect your arms and chest
The term is somewhat misleading because RLS doesn’t only affect your legs. This is a key reason for the ongoing effort to change the name of the condition from restless legs syndrome to Willis–Ekbom disease, named after two early scientists who studied the condition. As well as feeling discomfort in the legs (but rarely in the feet), some patients experience the same type of discomfort in their arms and chest.
3. If you kick in your sleep – it doesn’t always mean you have restless legs syndrome
Twitching or moving your arms or legs in your sleep is called periodic limb movement disorder (PLMD). Although the vast majority of people with restless legs syndrome have PLMD, the reverse isn’t true – many people who twitch or jerk their legs while sleeping don’t have restless legs syndrome. One key difference is that restless legs syndrome results in voluntary movement whereas PLMD is involuntary.
Several other issues can cause night-time leg movements
For those with periodic limb movement disorder (PLMD), night-time limb movements can be caused by secondary factors such as medications, or other underlying medical problems, such as Parkinson’s disease. But PLMD is also a syndrome in its own right. The exact cause of primary periodic limb movement disorder is unknown, although it has been linked to nerve abnormalities and is more common in middle-aged and older people. PLMD can also cause poor-quality sleep and daytime drowsiness.
Other sleep disorders that result in jerky leg movements include sleep-related leg cramps, which are similar to muscle cramps experienced during the day. Another condition is called sleep-related rhythmic movement disorder (SRRMD), which is mainly seen in children under five and normally involves movements such as t body rocking or leg banging. Leg movements are also associated with benign sleep myoclonus of infancy (BSMI), a movement disorder that starts in young babies and includes repetitive jerks of the limbs.
4. RLS may be caused by multiple factors – including genetics
The main causes of RLS are still unclear. However, research suggests that the interaction and combination of genetics and 2 other factors may trigger the onset of this disease:
- Broken dopamine signals: Images using special radioactive chemicals show that patients with severe RLS have reduced function of the dopamine receptors and transporters in their brains. Dr. Christopher Earley at the John Hopkins School of Medicine has used the analogy of a person watching TV to describe what may be happening in patients with RLS; when you can’t hear something clearly on TV, you turn up the volume; similarly, if a cell can’t “hear” the dopamine message from another cell, it tells it to turn up the dopamine.
- Brain iron deficiency: some evidence points to low iron levels in the brain as a cause of RLS, as it’s involved in many activities in brain cells, including dopamine. However, further research is needed to clarify how the brain can be low in iron while other organs in the body show normal levels, and why it leads to RLS.
- Genetics: 40-90% of people affected by RLS also have first-degree relatives suffering from this condition. Variations in 5 different genes have been linked to RLS, especially in families where symptoms start before the age of 40. It’s believed that these genes are involved in the development of neurons, but further research is needed to find out if these affect iron levels in the brain or in the dopamine signals.
While how those 3 factors interact is still unclear, other environmental factors may also trigger this disease:
- Certain medications to treat nausea, mental health disorders, colds, allergies, cardiovascular conditions or high blood pressure.
- Use of alcohol and caffeine
- Stress and anxiety
- Pregnancy, especially during the 3rd trimester
- Nerve damage
- Renal diseases
- Sleep deprivation and sleep disorders such as sleep apnea can also aggravate or trigger symptoms.
Is leg twitching at night an early sign of Parkinson’s Disease?
Some evidence suggests that this syndrome is related to a dysfunction in the basal ganglia, a section of the brain that controls movement through dopamine. This disruption of the dopamine pathways usually causes the involuntary movements that characterize Parkinson’s disease, which explains why many people with that disease also suffer from restless legs syndrome.
5. There are different home remedies and lifestyle changes that help relieve symptoms of RLS, both in adults and children.
As many people with restless legs syndrome already know, you can get some relief by treating yourself to a “spa-type” treatment at home or considering changes in your lifestyle. You can check them in detail in our article “8 home remedies for Restless Legs Syndrome”.
6. Babies and children can also suffer from Restless Legs Syndrome – but the diagnosis is still a challenge.
In the United States, approximately 1.5 million children and adolescents are estimated to have restless legs syndrome. About 35% of patients who report having RLS say it started before 20 years of age. However, diagnosing RLS in children may be especially difficult – sometimes misdiagnosed.
According to the Restless Legs Syndrome Foundation, children with RLS tend to seek relief from their discomfort by moving their legs – and the attempts to relieve the uncomfortable feeling may be viewed as hyperactivity or other disruptive behavior. In fact, the disease often results in symptoms that are very similar to those of ADHD and many children may receive this diagnosis. Moreover, the disruption in their sleep caused by the condition may result in irritability, fatigue or moodiness – complicating the proper diagnosis.
It’s essential to listen to the children when describing how it really feels and follow up when and how often they may complain, and for how long symptoms last. The remedies and changes in the lifestyle mentioned above may also apply to them.
7. There is also a link between RLS and pregnancy: about 1 in 5 pregnant women experience symptoms.
Pregnancy itself doesn’t cause RLS. However, it can lead to a combination of low iron levels and high estrogen levels that may trigger the onset of the condition. Typically, symptoms worsen as the pregnancy progresses, and it’s more common during the last trimester. Fortunately, RLS is only temporary for women who develop it during pregnancy – the symptoms usually go away within 4 weeks of delivery.
To help the condition during pregnancy, the same tips are recommended, especially those involving everyday regular exercise, relaxation techniques before bed to ensure enough and good quality sleep, massages in legs, feet and even arms, and applying heat or cold depending on how it makes you feel.
8. There isn’t a cure for RLS. But important discoveries are paving the way.
Right now, there is no known cure for restless legs syndrome, and no treatment options exist that work for everyone with RLS. Key medical treatment methods include medicines that target dopamine production, opiates (which have been used as a treatment for the condition since 1685), iron, certain types of sleeping pills (mainly benzodiazepines receptor agonists), and drugs that stabilize the electrical activity of nerve cells. However, new research is opening up new possible treatment alternatives. Research published in 2018 shows that targeting the way messages are sent between nerve cells may be a promising new path to finding treatments that could help prevent or alleviate the symptoms of RLS.